Salivary Gland Surgery
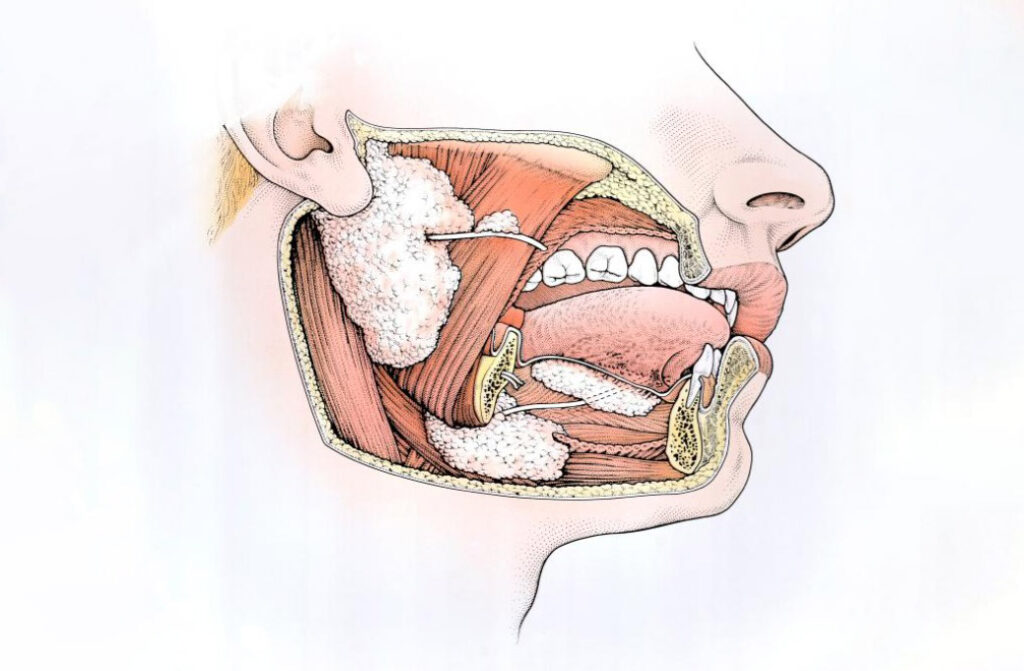
We have three pairs of major salivary glands: the parotid glands are in front of and below the ears, the submandibular glands are under the jaw bone, and the sublingual glands under the tongue in the mouth. There are also several hundred minor salivary glands throughout the mouth and throat. Examples of these minor glands can be felt as the small lumps inside the lower lip that can be felt with the tongue.
The most common reason for surgery of the salivary glands is to remove tumors. The tumors can be benign (noncancerous) or malignant (cancerous). Any of these glands can develop tumors, but most arise in the parotid glands. Other reasons for surgery are cysts, stones that form in the glands, chronic pain from inflammation, drainage of abscesses, and biopsy to diagnose other problems.
The Parotid Gland
The parotid gland is the largest salivary gland.It sits under the skin in front of the ear and extends into the upper neck behind the jaw. The parotid duct is a small tube that carries the saliva from the gland and into the mouth, opening inside the cheek, next to an upper molar tooth. An important aspect to the anatomy of the parotid gland is its relationship to the facial nerve, the nerve that goes to the face and causes all the facial movements and expressions—frowning, blinking, smiling, and closing the lips. Surgery puts this nerve at risk.
Eighty percent of parotid masses are benign. The cancers can be low grade, grow slowly, and less likely to spread (metastasize) to lymph nodes in the neck. But they can also be high grade, meaning aggressive, and grow quickly and spread readily to the neck nodes. These can also be quite painful. Surgery is usually recommended for any tumor for two reasons. First, the most common benign tumor, called a pleomorphic adenoma, can become a cancer. They are typically slow growing and can be present for years. Some estimate the risk of changing to a cancer is about 5% per year. These cancers are aggressive and need radical surgery. Second, as tumors get bigger the risks of surgery increase.
The surgery is called a parotidectomy. The incision is in front of the ear, curves below the ear and then extends into the neck. Most surgeries are done as an outpatient and people go home the same day. Larger tumors may require a drain be placed and removed a couple days later. Instructions are given for postoperative and drain care. Occasionally, the surgery is done in the hospital if the tumor is too large, the surgery is more complex, or other health problems require it. Treatment for cancer may require removal of lymph nodes from the neck and/or radiation therapy.
Risks of parotid surgery
- Bleeding. This may cause a collection of blood called a hematoma that needs to be drained
- Infection
- Weakness or paralysis of the facial muscles caused by damage to the facial nerve. Normally, this is only in single branches of the nerve and only affect a part of the side of the face, but it can affect the entire half of the face. Mild, temporary weakness can be seen in up to 10%. These almost always resolve after several days to weeks. Complete paralysis of a branch happens less than 5% of the time. These also have a good chance of recovery.
- Frey’s syndrome. Sweating in the area of the gland while eating
- Fluid collection under the skin. This can be serum (liquid caused by the trauma of surgery) or saliva from the cut gland. This can be drained with aspiration.
loss of tissue volume in front of the ear causing visible asymmetry - Numbness of the ear and cheek
- Scar
- Risks of general anesthesia
The Submandibular Gland
The main reason for removal of the submandibular glands is infection, chronic pain, obstruction of the duct, salivary stones. Sometimes tumors may develop in the gland. Fifty percent of tumors of the submandibular glands can be malignant. Surgery for removal of these glands requires a 4-5 cm incision under the jaw. The risks include bleeding, infection, damage to the marginal mandibular nerve causing paralysis to the lower lip, numbness or loss of taste to the side of the tongue, and scar. Sometimes a drain is placed, and some patients may need to stay the night in the hospital.
The Sublingual Glands
The sublingual glands are located under the tongue and rarely need to be removed. Unfortunately, 80% of the tumors that develop are malignant. A more common reason for removal is a ranula, which is a collection of mucous caused by a blockage of the duct. A ranula usually presents as a bluish or pink swelling under the tongue but can extend from the bottom of the mouth down into the neck, presenting as a soft, nontender lump under the jaw (called a “plunging ranula”. The sublingual glands are removed from under the tongue. Risks are bleeding, infection, scarring under the tongue, numb tongue or loss of taste, and blockage of the salivary duct of the submandibular gland.
Salivary Gland Conditions & Disorders
There are several conditions and disorders that can affect the salivary glands, here we will focus on the ones that may require surgery.
Sialadenitis
Infection or inflammation of the salivary glands is called sialadenitis. This can be caused by obstruction, bacteria, or viruses. Treatment is usually conservative and does not need surgery.
Conservative measures for sialadenitis are:
- Gentle massage of the gland to express saliva down the duct and relieve pressure
- Warm compresses applied to the affected gland
- Sialagogues—substances that cause salivation to flush the duct. I commonly recommend sugar free sour candy or a drop of lemon juice on the tongue.
- Adequate hydration to keep saliva thin
- Antibiotics as needed for infection.
Salivary Stones
Salivary gland stones develop from salts found in saliva and generally form due to dehydration or medications that cause dry mouth. These stones can lead to a blocked salivary gland, which is a painful condition that causes swelling and infection.
Tumors on Salivary Glands: Cancer
While most salivary gland tumors are noncancerous (benign), others can be malignant (cancerous). Benign tumors that can develop on a salivary gland include:
- Pleomorphic adenoma—most common benign tumor, but can change into a cancer
- Warthin’s tumor
- Oncocytomas
- Myoepitheliomas
- Other adenomas
Malignant, or salivary gland cancer, includes:
- Mucoepidermoid carcinoma—most common salivary gland cancer, can be low, intermediate, or high grade.
- Acinic cell carcinomas
- Polymorphous adenocarcinomas
- Salivary duct carcinomas
- Adenoid cystic carcinomas
- Carcinoma ex-pleomorphic (from a transformed pleomorphic adenoma)
- Metastatic skin cancer—skin cancer can spread to the lymph nodes in the parotid glands
Sialendoscopy
Sialendoscopy is a minimally invasive endoscopic technique to diagnose and treat salivary gland problems. A very small endoscope can be inserted into salivary ducts. The endoscope is outfitted with a light, a camera and tools. Tiny baskets and small graspers can extract very small salivary stones. Other tools can dilate blockages such as strictures of the salivary duct.
Indications
Salivary Stones
Salivary stones (sialolo (also called a sialolith) are mineral deposits that form in a salivary gland or duct. They can block the duct and cause pain, swelling and infection. Sialendoscopy can aid in the removal of a salivary stone.
Radiation-Induced Salivary Gland Damage
Radioactive iodine is used to treat some thyroid gland problems. The salivary glands can take up the radioactive iodine and be damaged by it. This is more common in high doses. Sialendoscopy can be used to dilate the damaged ducts, flush out debris, and inject steroids into the gland.
Chronic Salivary Gland Infection
Sialendoscopy can be used to dilate the damaged ducts, flush out debris, and inject steroids into the gland.
What to Expect
- Before performing a sialendoscopy, the doctor may order imaging studies such as a computerized tomography (CT) scan, magnetic resonance imaging (MRI) or ultrasound to look at the salivary gland that is causing problems.
- You will receive general anesthesia. Follow your doctor’s instructions on eating, drinking and taking your regular medications before the sialendoscopy.
- The doctor will guide the endoscope into the duct of the salivary gland in your mouth. If the opening is too tight, it may be gently stretched to accommodate the scope.
- The doctor will use the endoscope to rinse (irrigate) the inside of the gland with saline to remove debris.
- Using the light, camera and tools with the endoscope, the surgeon inspects the interior of the gland, and then removes salivary stones and addresses blockages.
- In some cases, the doctor may recommend a sialendoscopy together with traditional open surgery to provide a better view and gain access to the inside of the salivary gland.
- Sometimes, the surgeon may need to leave a stent in the duct for a prolonged period to prevent scarring and blockage.

Sialendoscopy Risks and Complications
Because sialendoscopy is minimally invasive, there may be less risk of complications than with traditional, open surgery on the salivary gland. However, though rare, sialendoscopy complications are possible and include:
- Strictures (tightening of the duct)
- Perforation of the duct
- Bleeding
- Ranulas, which are benign cysts filled with saliva
Request an Appointment
Same and next day appointments available
